Massive ingestion of toxic products (alcohol, diets rich in fat or sugars, aromatic chemical molecules...) or infection by hepatitis viruses leads to liver fibrosis. This pathology is characterized by an accumulation of connective tissue in the liver that interferes with its physiological functions. Liver fibrosis can progress to more severe degradation called cirrhosis. During this pathological evolution, the
endothelium of the hepatic blood capillaries undergoes a transformation called capillarization during which it loses its properties as a porous barrier between blood and hepatocytes. What cellular and molecular processes are then involved?
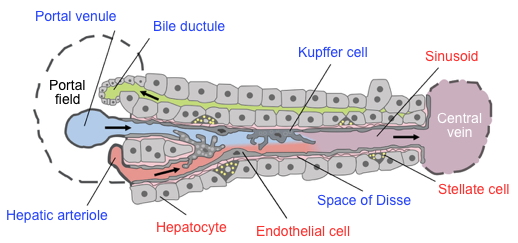
The liver performs many vital functions including blood detoxification, vitamin synthesis, carbohydrate, fat and protein metabolism, and bile production which is essential for digestion. Crossed every minute by 1.4 liters of blood, the liver is one of the most densely vascularized organs. It receives blood from two major vessels: the hepatic artery which carries oxygenated blood, and the portal vein which carries low-oxygenated blood that is enriched in substances from the stomach, intestines, spleen and pancreas, which will be transformed as they pass through the liver. As they penetrate the liver, the hepatic artery and portal vein divide into a network of capillaries called hepatic sinusoids (
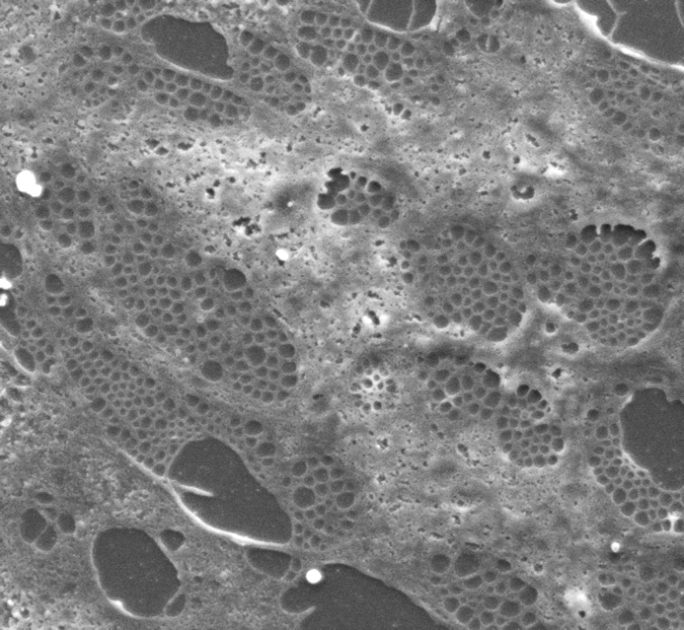
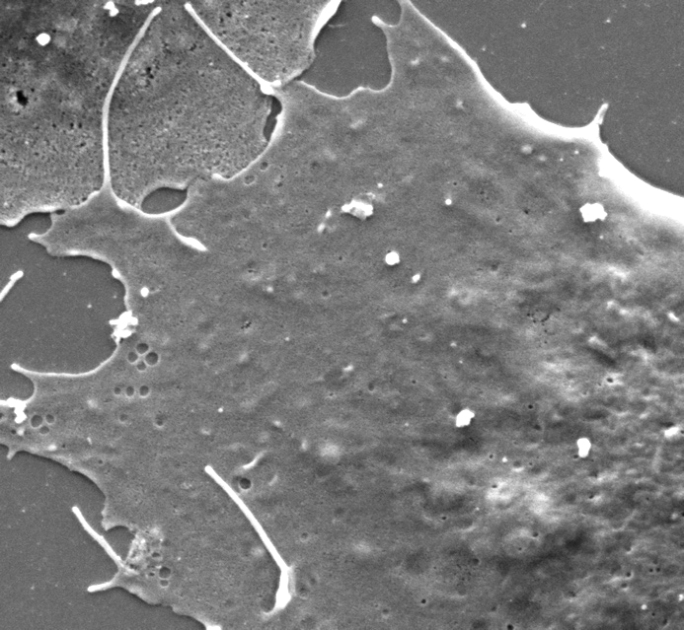
Figure). The endothelial cells that cover the inside of these hepatic sinusoids have very specific properties that distinguish them from the endothelial cells from other organs. They are perforated by fenestrae with an approximate diameter of 100 to 150 nm that facilitate communication between circulating blood and hepatocytes located on either side of this endothelial barrier. They also have
endocytosis receptors and so called scavenger receptors on their surface to clean the blood of toxic agents, cell debris and any bacterial contaminants it carries.
Researchers at our Laboratory have been studying the
cytokine BMP9 (
Bone Morphogenetic Protein 9) for several years and have identified it as the very high affinity ligand of the ALK1 receptor (
Activin receptor-Like Kinase 1). ALK1 is expressed almost exclusively by endothelial cells while BMP9 is synthesized and secreted by stellate cells in the liver (
Figure). In a recent study, these researchers studied the phenotype of a mouse strain (129/Ola) in which the gene encoding BMP9 was deleted. These mice appear to have a normal embryonic life but develop significant perivascular hepatic fibrosis after 15 weeks of adult life. A detailed histological and molecular analysis of their hepatic blood vessels showed that the endothelial cells of their hepatic sinusoids have very few fenestrae and are capillarized (
Figure). Capillarization is defined not only by the loss of fenestrae but also by the loss of expression of scavenger and the endocytic properties of liver endothelial cells.
Surprisingly, mice of another strain (C57/Bl6) whose
BMP9 gene has also been deleted do not develop hepatic fibrosis, suggesting that a genetic factor protects them from this anomaly.
| |
|
| | |
Normal liver sinusoid endothelial cell | | Liver sinusoid endothelial cell in the absence of BMP9 |
Credit: Agnès Desroches-Castan and Emmanuelle Tillet
Taken together, these studies indicate that BMP9, produced by stellate cells in the liver, acts as a
paracrine factor on sinusoidal endothelial cells by promoting maintenance of fenestration and preventing hepatic fibrosis. This observation positions the BMP9/ALK1 signaling pathway as a novel actor in hepatic physiology and as a therapeutic target for the treatment of hepatic fibrosis.
Hepatic structure. Originally by Frevert U, Engelmann S, Zougbédé S, Stange J, Ng B,
et al. Converted to SVG by Viacheslav Vtyurin who was hired to do so by User: Eug. [
CC BY 2.5],
via
Wikimedia Commons.
The vascular
endothelium is the innermost layer of the blood vessels, the one in contact with the blood.
Endocytosis is the mechanism of transport of molecules or even particles (viral, bacterial, etc.) to the inside of the cell.
Cytokines are soluble cell signaling substances that act remotely on other cells to regulate their activity and function. Their action, through specific receptors, can be
paracrine (close cells), endocrine (distant cells or tissues), juxtacrine (cells in contact) or autocrine (on the producing cell or a similar close cell).